Beyond COVID-19: Diseases that Plague Africa

Amanda Betag,1Thank you to Aransi Waliyi Olayemi, Nadir Al Kharusi, Cornelius Apungwa, Alex Kopytko, Kenneth Dickhudt, Dr. John Marangos, Liam Palmbach, and Dr. Robin Hardy, fellow members of the Africa Center for Strategic Progress, for their feedback and comments on this article. Research Fellow, African Political Economy Lab
abetag@africacfsp.org
COVID-19 has affected nations worldwide, and Africa has been no exception. However, the focus cannot be removed from other diseases that continue to plague millions of African citizens. Prevention and treatment programs for malaria, tuberculosis (TB), and HIV/AIDS have been severely affected due to the increased attention on fighting the pandemic, leaving these diseases the ability to run rampant. This article reviews recent research that estimates the total impact of the reduction in programs targeted at these other diseases.
Introduction
COVID-19 has been rapidly growing across Africa, becoming the biggest concern for the continent. However, there are still other diseases that plague Africa. COVID-19 has the potential to impede the treatment of other diseases by shifting resources away to focus on the pandemic, especially in low-income countries where resources are already limited. This article discusses the need for countries to continue to treat diseases other than COVID-19 present in the area. Most notably, malaria, tuberculosis (TB), and HIV/AIDS torment most African countries and create huge economic burdens in terms of foregone economic growth for these countries.
Malaria
According to the 2019 World Malaria Report, there were an estimated 228 million cases of malaria worldwide, with 93 percent, or 213 million, of these cases occurring in Africa in 2018.2World Health Organization (WHO), The. “World Malaria Report 2019.” World Health Organization, December 4, 2019. https://www.who.int/publications/i/item/world-malaria-report-2019. This report also documented an estimated 405,000 deaths from malaria globally, with 94 percent of deaths occurring in Africa.3See note 2. Those who are at the greatest risk of dying from malaria are children under the age of five, who accounted for 67 percent of all malaria deaths worldwide.4See note 2.
With COVID-19 as the primary focus of most countries’ health services, these figures are expected to increase significantly. The World Health Organization (WHO) analyzed nine scenarios which investigated the extent of the malaria epidemic’s disruption on a country’s health services. In the worst-case scenario, there would be no insecticide-treated net (ITN) campaigns and both continuous ITN distributions and access to effective antimalarial treatment were reduced by 75 percent. Depending on the scenario, the WHO estimates an additional 15 to 46 million additional cases of malaria in sub-Saharan Africa with an additional 50,000 to 318,000 deaths.5World Health Organization (WHO), The. “The potential impact of health service disruptions on the burden of malaria: a modelling analysis for countries in sub-Saharan Africa.” World Health Organization, April 23, 2020. https://www.who.int/publications/i/item/the-potential-impact-of-health-service-disruptions-on-the-burden-of-malaria” https://www.who.int/publications/i/item/the-potential-impact-of-health-service-disruptions-on-the-burden-of-malaria.
Moreover, 70 percent of these deaths would be among children under the age of five.6See note 5. The complete estimates from this report are summarized below in Table 1.7See note 5.
Table 1: Estimated Excess Cases and Deaths from Malaria in sub-Saharan Africa
Scenario | Excess Cases | Excess Deaths |
Scenario 1 | 15,303,942 | 25,241 |
Scenario 2 | 17,574,789 | 29,081 |
Scenario 3 | 18,802,981 | 31,148 |
Scenario 4 | 8,857,461 | 101,460 |
Scenario 5 | 17,883,653 | 210,971 |
Scenario 6 | 27,059,774 | 328,748 |
Scenario 7 | 25,233,210 | 134,487 |
Scenario 8 | 35,809,832 | 253,724 |
Scenario 9 | 46,358,814 | 382,145 |
Source: World Health Organization (WHO), The. “The potential impact of health service disruptions on the burden of malaria: a modelling analysis for countries in sub-Saharan Africa.” World Health Organization, April 23, 2020.
It is also important to note that some countries would be more affected than others. For instance, not all countries are scheduled to have ITN campaigns, which typically occur every three years. Therefore, only countries that were due for ITN campaigns in 2020 would be affected by their cancellation. Additionally, the seasonality of malaria is different in every country, with peaks occurring at various times depending on the country or region. For example, malaria cases peak in February in Zambia, but do not peak until September in Niger. Therefore, countries that experience peaks during the height of COVID-19 will be at greater risk of higher cases and deaths from malaria. According to the WHO’s analysis, the countries expected to experience the greatest percentage increases in deaths from malaria under the worst-case scenario include Angola, Côte d’Ivoire, Gabon, Gambia, Ghana, Guinea-Bissau, Kenya, Liberia, Mozambique, Namibia, Nigeria, Rwanda, South Africa, Togo, Uganda, the United Republic of Tanzania, Zambia, and Zimbabwe, all of which are predicted to have a 100 percent or greater increase in deaths in this scenario.8See note 5.
Tuberculosis
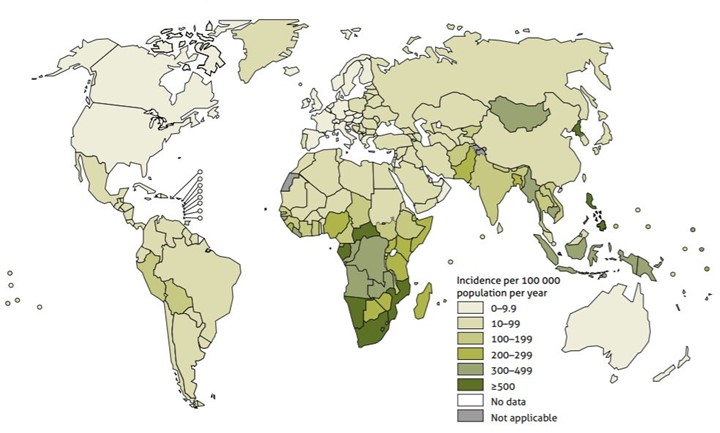
In Africa, 2.5 million people were infected with tuberculosis (TB), accounting for a quarter of new TB cases worldwide, and an estimated 417,000 people died from the disease in 2016.9World Health Organization (WHO), The. “WHO Africa, Health Topics, Tuberculosis (TB).” World Health Organization, 2020. https://www.afro.who.int/health-topics/tuberculosis-tb#:~:text=In%202016%2C%202.5%20million%20people,occur%20in%20the%20African%20Region. Additionally, over 25 percent of TB deaths occur in Africa.10See note 9. Figure 1 depicts the estimated TB incidence rates in 2018 across the world and shows that many of the countries with the highest incidence rates are in sub-Saharan Africa.11World Health Organization (WHO), The. (2019, Oct 17). Global Tuberculosis Report 2019. World Health Organization. Retrieved on July 25, 2020 from https://www.who.int/tb/publications/global_report/en/
Figure 1: Estimated TB Incidence Rates, 2018
An analysis by the Stop TB Partnership, which aims to make tuberculosis a high priority on the global political agenda, investigated how COVID-19 would affect the treatment of TB in high-burden countries, many of which are in Africa, by focusing on two possible scenarios. Under the best-case scenario, there would be a two-month lockdown with a two-month recovery, and, under the worst-case scenario, there would be a three-month lockdown with a ten-month recovery. Under these scenarios, they estimate a 3.1 to 10.7 percent increase in cases and a 4 to 16 percent increase in deaths from 2020 to 2025.12Stop TB Partnership. “The potential impact of the COVID-19 response on tuberculosis in high-burden countries: a modelling analysis.” Stop TB Partnership, July 13, 2020. http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf. In other words, there would be an estimated 1.8 to 6.3 million additional cases and 340,000 to 1.4 million additional deaths from TB worldwide.13See note 12. Since 25 percent of all new TB cases originate in Africa and 25 percent of TB deaths occur in Africa, this analysis would imply roughly 450,000 to 1.6 million additional cases and 85,000 to 350,000 additional deaths in Africa alone.14See note 9.; See note 12. Lastly, the Stop TB Partnership estimated the amount of additional cases and deaths for every month of lockdown and for every month of recovery. These results, after taking 25 percent of the total estimated number of cases in deaths in Africa into account, are summarized below in Table 2.15See note 12.
Table 2: Estimated Excess Cases and Deaths from TB in sub-Saharan Africa
Scenario | Excess Cases | Excess Deaths |
For every month of lockdown | 152,100 | 31,525 |
For every month of restoration | 105,100 | 20,800 |
Source: Stop TB Partnership. “The potential impact of the COVID-19 response on tuberculosis in high-burden countries: a modelling analysis.” Stop TB Partnership, July 13, 2020.
There is also the question of whether COVID-19, through the physical distancing measures taken, could actually improve the TB situation in Africa. Furceri et al. (2020), a group of researchers from the International Monetary Fund (IMF), evaluated this situation by creating a model based on data from three of the most high-burden countries in the world; China, India, and South Africa. They concluded that any potential benefit from physical distancing would likely decrease TB incidence far more than it would decrease TB deaths.16David Furceri, Prakash Loungani, Jonathan D. Ostry, and Pietro Pizzuto. “Will Covid-19 affect inequality? Evidence from past pandemics.” Centre for Economic and Policy Research, COVID Economics Vetted and Real-Time Papers, 12: 138–157, May 1, 2020. They also concluded that any benefit, if present at all, would likely be outweighed by the disruption in health services.17See note 16. Therefore, although the figures presented by the Stop TB Partnership may be an overestimate since it did not factor in the potential benefits of social distancing, it is nonetheless likely that TB cases and deaths will remain high due to health service disruptions. Both these papers agree that it is crucial to maintain and strengthen TB-related health services during and after the COVID-19 pandemic.
HIV/AIDS
As of 2016, HIV/AIDS is the second leading cause of death for people in Africa.18World Health Organization (WHO). “Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2016.” World Health Organization, 2018. Africa is also the most affected continent in the world, with 25.7 million people living with HIV in 2018.19World Health Organization (WHO), The. “WHO Africa, Health Topics, HIV/AIDS.” World Health Organization, https://www.afro.who.int/health-topics/hivaids. HIV is most pronounced in Eastern and Southern Africa, followed by Central and Western Africa. Africa also accounts for almost two thirds of the global total of new HIV infections.20See note 19. With the prevalence of HIV in Africa, COVID-19 poses a great threat to the treatment of HIV/AIDS and could cost many more people their lives.
One analysis funded by the Bill & Melinda Gates Foundation estimated the potential effects of COVID-19 on HIV by estimating the relative change in HIV incidence and mortality from six-month disruptions in different prevention programs, HIV testing, and treatment and care. They used five different mathematical models for disruptions of 20, 50, and 100 percent over a one-year period. Additionally, they estimated the excess HIV-related deaths over a one-year period due to a six-month disruption in a number of sub-Saharan African countries, different African regions, and for sub-Saharan Africa as a whole using the same five models. They found that, in sub-Saharan Africa, a 20 percent disruption could lead to between 92,299 and 150,000 excess deaths, a 50 percent disruption could lead to between 229,023 and 420,000 excess deaths, and a 100 percent disruption could lead to between 461,682 and 956,600 excess deaths.21Britta L Jewell, Edinah Mudimu, John Stover, Debra ten Brink, Andrew N Phillips, Jennifer A Smith, Rowan Martin-Hughes, Yu Teng, Rob Glaubius, Severin Guy Mahiane, Loveleen Bansi-Matharu, Isaac Taramusi, Newton Chagoma, Michelle Morrison, Meg Doherty, Kimberly Marsh, Anna Bershteyn, Timothy B Hallett, and Sherrie L Kelly. “Potential effects of disruption to HIV programs in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models.” The Lancet, August 6, 2020. https://doi.org/10.1016/S2352-3018(20)30211-3. Furthermore, they showed that Eastern and Southern Africa would be hit much harder than Western and Central Africa. For example, for a 50 percent disruption in services, Eastern and Southern Africa is estimated to have an excess of 186,000 to 320,000 deaths compared to Western and Central Africa, which is predicted to have an excess of 32,134 to 100,800 deaths.22See note 21. These estimates, as well as further estimates for the different regions of Africa, are summarized in Table 3.23See note 21.
Table 3: Estimated Excess Deaths from HIV in sub-Saharan Africa
Scenario | Excess Deaths in sub-Saharan Africa | Excess Deaths in Eastern and Southern Africa | Excess Deaths in Western and Central Africa |
20% Disruption | 92,299 – 150,000 | 77,000 – 110,000 | 12,950 – 40,000 |
50% Disruption | 229,023 – 420,000 | 186,000 – 320,000 | 32,134 – 100,800 |
100% Disruption | 461,682 – 956,600 | 351,000 – 700,600 | 64,778 – 256,000 |
Source: Britta L Jewell, Edinah Mudimu, John Stover, Debra ten Brink, Andrew N Phillips, Jennifer A Smith, Rowan Martin-Hughes, Yu Teng, Rob Glaubius, Severin Guy Mahiane, Loveleen Bansi-Matharu, Isaac Taramusi, Newton Chagoma, Michelle Morrison, Meg Doherty, Kimberly Marsh, Anna Bershteyn, Timothy B Hallett, and Sherrie L Kelly. “Potential effects of disruption to HIV programs in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models.” The Lancet, August 6, 2020.
Effect on Economic Growth
All of the analyses in this paper lead to one conclusion: if health services are discontinued during and/or after the COVID-19 pandemic, there will be many lives lost. Not only this, but lacking health services would also have detrimental effects on the economies of many African countries, especially sub-Saharan Africa.
Over the years, sub-Saharan Africa has seen immense growth, but this is set to change in the coming year.24World Bank. “The Work Bank in Africa.” The World Bank, April 23, 2020. https://www.worldbank.org/en/region/afr/overview#1. In fact, sub-Saharan Africa is expected to see its first recession in 25 years due to COVID-19.25See note 24. Although most of the decrease in growth is expected to be due to the pandemic, the increase in malaria, TB, and HIV/AIDS would also likely decrease economic growth in a similar manner that COVID-19 has done. For example, an increase in the incidence and deaths from malaria, TB, and HIV/AIDS is expected to decrease growth through lower worker productivity, reduced labor supply, decreased resources going towards things such as education and public investments, decreased tourism, and decreased savings at the societal level, according to a number of studies.26Simon Dixon, Scott McDonald, and Jennifer Roberts. “The impact of HIV and AIDS on Africa’s economic development.” BMJ, January 26, 2002. https://doi.org/10.1136/bmj.324.7331.232; John Luke Gallup and Jeffrey D. Sachs. “The Economic Burden of Malaria.” The American Journal of Tropical Medicine and Hygiene, 64(1): 85-96, January 1, 2001. https://doi.org/10.4269/ajtmh.2001.64.85.; Franque Grimard and Guy Harling. “The Impact of Tuberculosis on Economic Growth.” Department of Economics: McGill University, 2004. https://www.semanticscholar.org/paper/THE-IMPACT-OF-TUBERCULOSIS-ON-ECONOMIC-GROWTH-Grimard-Harling/5f20d9c60efa43dd38fe284792bed2d529e6c000#citing-papers.; Ramanan Laxminarayan, Eili Klein, Christopher Dye, Katherine Floyd, Sarah Darley, and Olusoji Adeyi. “Economic Benefit of Tuberculosis Control.” The World Bank, policy research working paper 4295, August 2007. http://documents1.worldbank.org/curated/en/554871468175465282/pdf/wps4295.pdf.; Enrico Lovász and Bernhard Schipp. “The Impact of HIV/AIDS on Economic Growth in sub-Saharan Africa.” Wiley Online Library, June 4, 2009. https://doi.org/10.1111/j.1813-6982.2009.01210.x.; Nayantara Sarma,Edith Patouillard, Richard E. Cibulskis, and Jean-Louis Arcand. “The Economic Burden of Malaria: Revisiting the Evidence.” The American Journal of Tropical Medicine and Hygiene, 101(6): 1405-1415, December 2019. http://www.ajtmh.org/content/journals/10.4269/ajtmh.19-0386. The reduction in growth can also be forecasted from the known relationship between health and economic growth. Many studies show that good health and investing in a healthier population is essential for growth and that diseases that plague many countries are responsible for a significant amount of foregone growth.27Alok Bhargava, Dean T. Jamison, Lawrence Lau, and Christopher JL Murray. “Modeling the Effects of Health on Economic Growth.” Journal of Health Economics, 20(3): 423–440, May 2001. https://doi.org/10.1016/S0167-6296(01)00073-X.; David E. Bloom, David Canning, and Jaypee Sevilla. “The Effect of Health on Economic Growth: Theory and Evidence.” World Development, 32(1): 1–13, 2004. https://doi.org/10.1016/j.worlddev.2003.07.002.; David E. Bloom, Michael Kuhn, and Klaus Prettner. “Health and Economic Growth.” IZA Institute of Labor Economics, discussion paper 11939, November 2018. http://ftp.iza.org/dp11939.pdf.; Julio Frenk. “Health and the economy: A vital relationship.” OECD Observer, May 2004. https://oecdobserver.org/news/archivestory.php/aid/1241/Health_and_the_economy:_A_vital_relationship_.html#:~:text=A%20strong%20relationship.,on%20the%20health%20systems%20themselves.&text=Investment%20in%20health%20is%20not,essential%20priority%20for%20most%20societies..; World Health Organization. “WHO Guide to Identifying the Economic Consequences of Disease and Injury.” World Health Organization, 2009. https://apps.who.int/iris/handle/10665/137037. Therefore, there is extensive evidence showing that the increase in malaria, TB, and/or HIV/AIDS would further hamper economic growth in Africa.
Conclusion
It is not only necessary for the sake of saving lives, but continuing prevention programs and treatment for malaria, TB, and HIV/AIDS is also vital for Africa’s economic growth. It is easy to lose sight of these diseases while the world is facing a pandemic, but doing so will have catastrophic consequences that will be seen for many years to come. It is worth directing the available resources today towards these services to prevent even further costs in the future.
Based on your interests, you may also wish to read:
- How Can Sub-Saharan African Countries Minimize the Impact of Coronavirus Pandemic on Economic Performance?
- Africa, COVID-19, and the International Financial Institutions
- Restarting Growth in Countries with Ongoing Conflicts After Covid-19
- To Benefit from the Belt & Road Initiative, Africa Needs a Unified Approach


